A brain injury can alter life forever, for the person who sustains the injury as well as those in a relationship with that person. The more you know about brain injury the more confident you will be in your ability to cope with these changes and find effective ways to manage the challenges that follow.
Get the Facts!
There's always something new to learn about brain injury. Getting our facts straight is a crucial first step in moving toward the best possible outcomes.
TBI Facts:
Myth: Knowing which parts of the brain have been injured will tell you the specific challenges to expect.
Fact: By knowing the location of the injury to the brain, you may have some indication of the problems to expect but not to the point of being able to predict specifically what lies ahead. Every response to brain injury is different.
Myth: Many people can’t change their behavior after a brain injury.
Fact: With proper support and therapeutic intervention, many people with brain injury have the ability to change their behavior, learn new things, and lead full and productive lives.
Myth: The best way to help a person with brain injury is to assist them with tasks.
Fact: As a parent, sibling or spouse of an adult with brain injury, general wisdom suggests that you be there to assist when needed, but avoid offering assistance for activities that can be done independently. Overriding your family member’s efforts (such as jumping in to finish sentences or tasks) lessens a personal sense of dignity, respect and self-worth.
Myth: After a brain injury, a person’s basic emotional needs change.
Fact: People with brain injury have the same emotional needs as every other person: to feel loved, to feel useful, to feel needed, to be treated with respect and to exercise control over their lives.
Myth: Personality traits often change significantly after a brain injury.
Fact: Actually, personality traits tend to intensify (become stronger) after a brain injury A mild mannered person may tend to become more mild mannered. An aggressive personality may tend to become more difficult and more aggressive after brain injury.
Myth: Most recoveries for brain injury show steady improvement up until 2 years when recovery is complete.
Fact: There will be inconsistency during the recovery period. A person with a brain injury may be able to do something easily one day, then find the same thing difficult the next day. Although much of the recovery process occurs during the first two years, it is not necessarily complete in 2 years. Recovery can continue throughout a lifetime.
Myth: The amount of time the person with a brain injury remains in a coma is the main factor that affects recovery.
Fact: The amount of time in a coma is one of many factors that will affect recovery. Other factors are:
- age,
- severity of the injury,
- where in the brain the injury is located,
- early patterns of recovery,
- length of time a person is very confused or experiences amnesia,
- other injuries to the body, and
- the level of health before the injury.
In the following videos, Tim Feeney, PhD, a nationally recognized rehabilitation expert, disscusses issues that many families face after a loved one sustains a brain injury.
Click on the title of each section to view or hide the content.
-
Now What?
-
Recovery from brain injury is a lifelong journey. The recovery process is as unique as the individual who has sustained the injury.
What can I do to help recovery?Support from family and friends is a big factor in the recovery and quality of life for individuals with brain injury. The challenges that come with brain injury provide opportunities to learn and grow. Relationships can strengthen. People with brain injury and their families can lead full and productive lives.
-
Care for the Caregiver
-
Caring for your family member can be emotionally and physically exhausting. In the midst of everything, it’s typical to wrestle with a wide assortment of emotions, such as guilt, anger, and grief.Tips for Coping
- Express your feelings. Find a way to “vent” when you are feeling down or frustrated. Bottled up emotions will not go away; they will only get stronger and create more stress. You can share your feelings by talking with others, or you can express them by writing in a journal, playing music, or doing artwork. Choose the method that works best for you.
- Talk with a friend. An old Swedish proverb says, Shared joy is a double joy; shared sorrow is half a sorrow. Talking with a caring friend can help relieve sadness and help you regain perspective. Find someone who will listen without making judgments or giving advice.
- Talk with others in a similar situation. People who are “in the trenches” know exactly what it is like. A support group for caregivers or families provides a safe and supportive place to share feelings. Members often share tips and resources for handling problems, which is an added benefit.
- Take a break. If you are feeling overwhelmed by feelings of grief, try to take a break. Take ten minutes, half an hour, or whatever you need to work through your emotions. It also helps to do something to express your feelings. Find a private place and cry, call a friend, write, or draw. Do anything to release the buildup of emotions so you can think more clearly. Or, do something physical during your time out. Activity is often a good way to reduce the intensity of built-up emotions.
- Be physically active. Vigorous activity speeds up your body’s metabolism. This can help decrease feelings of sadness. You do not have to be an athlete to get in some physical activity. Just taking a walk several times a week is enough to make a significant difference in your emotional health.
- Take time. There is no fixed path or timetable for your grief. Take time to work through your feelings about what has happened and how it has affected you and your family. Do not minimize what has happened and don’t let others underrate your loss. It is real and so are your feelings.
- Ask for help. You do not have to do this alone. Friends and family can be great sources of comfort and strength. There are times when more help is needed from someone who is not directly involved who can guide and counsel you. Consider talking with a clergy person, counselor, social worker, or psychologist who understands and has experience with families and brain injury.
- Express your feelings. Find a way to “vent” when you are feeling down or frustrated. Bottled up emotions will not go away; they will only get stronger and create more stress. You can share your feelings by talking with others, or you can express them by writing in a journal, playing music, or doing artwork. Choose the method that works best for you.
-
Communication
-
What is Effective Communication?Saying exactly what you mean is a good first step, but effective communication occurs only when a message is actually understood as it was intended. And that can be difficult, especially when communicating with someone with a brain injury.
Communication is a complicated chain of events that requires hearing, perceiving, remembering, understanding, processing, thinking, taking turns, and an array of abilities – all controlled by the brain.
When talking with someone with a brain injury, it is likely that you will need to make some adjustments in the way that you communicate. There are many strategies to help. The following 3 tips are a good place to start.
- Choose the right time
- Timing is everything when communicating with a person with brain injury. When important issues or conflicts arise, choosing the right time can increase the likelihood of a successful conversation.
Is now the time to talk? Ask yourself: Are both you and your conversation partner: Rested? Calm? Able to focus?
-
Once you have found a good time to talk, the next step is to choose what issues to talk about. There can be many challenges when living with a person with brain injury and it can be overwhelming to try to talk about everything. That’s why it is important for you to pick just a few areas to work on at a time.
- Timing is everything when communicating with a person with brain injury. When important issues or conflicts arise, choosing the right time can increase the likelihood of a successful conversation.
- Set the stage, then engage
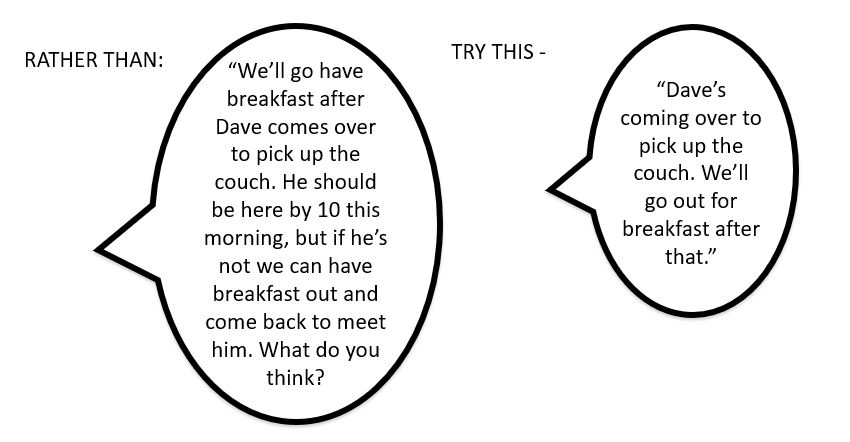
- When a person has memory and organizational challenges, avoid asking a lot of questions.
- Set the stage. Start with a simple sentence.
“Your sister is coming this weekend.” -
Then engage. Give information related to the topic.
“Last time she was here, you and she took some nice walks together.”
OR
Encourage further action.
“Let’s email your sister about our plans for her visit.”
- Keep it simple.
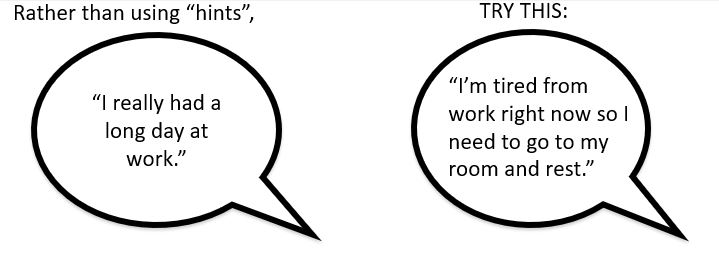
- TBI can slow the speed of thinking, comprehension, and the ability to process information. Jokes, words with double meanings, and complex sentences can be hard to understand.
- Limit words and details.
- Be Direct. Brain injury makes it difficult to understand abstract language (jokes, sarcasm, words with double meanings) or “hints” (comments with expected understanding.) Be straight forward.
Learn more about effective communication from the following video with Dr. Feeney.
- Choose the right time
-
What's in Your ToolBox?
-
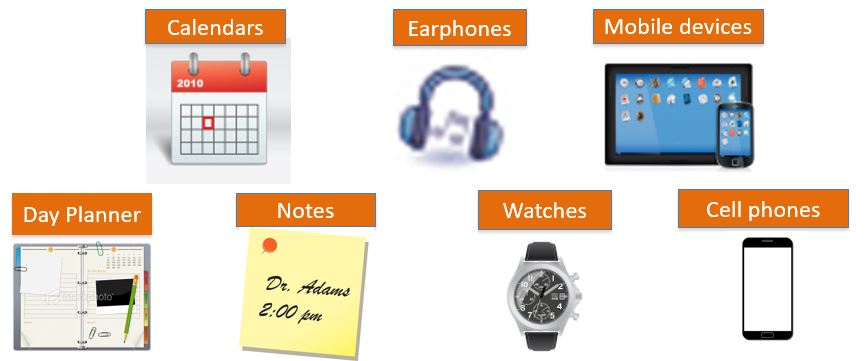
The Brain Changes after an Injury.Brain injuries can change one’s ability to :
- organize and plan
- remember dates, times, how to do things
- get started on tasks or activities
Tools can Help.
Support tools help individuals with brain injury compensate for the cognitive challenges that may occur after injury. Some people prefer paper and pencil tools such as notepads, memory books, post-it notes and calendars. Other people prefer to use electronic tools such as watches, tablets or smartphones, as well as auditory tools such as earphones.Choose the right tool!
Talk with your family member to be clear about needs, skill level, preferences and budget before selecting any tool.When selecting a tool consider:
- Does it meet our needs?
- Does it match the user’s skill level?
- Does it satisfy the user’s likes and level of comfort?
- Does it fit our budget?
- Does it need to travel with the user or stay in one place?
Give it Time.
- Allow your family member plenty of time to try out the tool. It takes time to learn to use a support tool effectively and determine if it is the best tool for the intended task.
- You may need to re-teach how to use the tool several times. There will be days when your family member looks like he or she has got it, and then the next day isn’t sure how to use the tool.
- With time, teaching, practice, review and lots of patience your family member may find an appropriately selected tool to be a great support.
- If the tool isn’t working after giving it both time and effort, try something else.
-
The Home Environment
-
Making Home that Quiet PlaceA calm, less stimulating home environment provides a supportive setting for someone with a brain injury.
A supportive environment can:
- Reduce memory and attention challenges
- Prevent headaches
- Decrease frustration and agitation
- Decrease fatigue
- Making simple changes in your home can help to calm the environment.
How are Things at Your House?

Does your family member have any of these common sensitivities?- fluorescent lights
- background noise (TV or radio when no one is listening)
- clutter
- loud noises
Small Changes Can Make a Difference. You can help.
Many people with brain injury are bothered by light.- Use lamps instead of overhead lighting; use lower level bulbs in the lamps.
- Replace fluorescent bulbs if they cause headaches.
- Use dimmer switches on lamps.
- Close curtains or blinds.
If noise is an issue, try to:
- Turn down, turn off, or move TV to a smaller room.
- Encourage family members to lower voices.
- Encourage the use of headphones or ear buds to block noise when needed.
- Set phones to vibrate instead of ring.
- Calm the barking dog or send it to another part of the house or outside.
- Arrange for scheduled quiet times at home.
- Go to the mall or restaurants at times that are less busy, less crowded.
Reduce clutter:
- Simplify surroundings by having fewer items in rooms and on surfaces.
- Clear tabletops and workspaces.
- Stack or store papers, books and magazines in containers or files.
- Fold and put away clothes, blankets, toys.
- Keep pathways clear and free of clutter.
Make it easy to find things:
- Keeping items in the same place
- Arrange everyday items in a consistent way. Examples: milk is always on the right top shelf, keys are always hanging next to the door…
- Put frequently used items in one, easy-to-see place (hang on a pegboard or put on a shelf.
- Be sure to post important names and phone numbers in one, convenient place.
If locating items is difficult, try to:
- Label drawers, cupboards and closets if needed (bedroom, kitchen, basement) with the name or pictures of the contents –“silverware”, “socks”, “tools” . . .
- Post a bulletin board with important phone numbers, appointments, and notes
- Remember, if you move where the item is kept, move the label too!
You can work with your family to calm your home environment and make life a little easier for your family member with a brain injury.
- A little less noisy, bright and cluttered.
- And full of reminders and helpers and organization tools for remembering and finding important items.
With your family member, think about environmental changes that might be helpful in your home. Make a list!
Ideas for making physical changes:
- Turn off noisy devices when not in use
- Clear clutter from rooms
- Use natural lighting when possible or lamps instead of florescent or overhead lights
- Label drawers and cupboards in areas of difficulty
- Keep workspaces organized and uncluttered
- Remove distractions
- Organize frequently used items in areas where they can be seen
Good intentions work best when put into a workable plan. Complete your plan by adding the WHO and the WHEN to each item.
-
Creating Routines Using Lists and Schedules
-
Daily Activities and Routines
We all have routines for daily activities and chores. Often we don’t even have to think about how to do them – we can do them on “autopilot”.
These routines and habits help us do the things we need to without exerting a lot of mental energy.Routines:
- Provide structure for day-to-day activities
- Improve a person’s ability to complete tasks
- Reduce frustration
Loss of habits and routines
Brain injuries can affect the ability to remember how to follow a routine, or to put the steps of a routine in the correct order.
Not being able to do things by habit anymore is frustrating for your family member. And it is likely time-consuming and frustrating for you too.For someone with a brain injury, getting from Point A to Point B, even if it is a regular activity or chore, can be difficult.
Using a simple tool – a well-written list of steps – can be very helpful, replacing a routine or habit, providing a sense of accomplishment and giving more freedom and independence.
What does your family member most want to do that can be helped by a list? Work together to decide.
Here are the basic steps:
- Identify the starting point.
- Do the process yourself a step at a time.
- Check the steps by following your own written list. Adjust as needed.
- Have your family member try it out. Adjust as needed.
Tip:
You might think that you can create the list from memory, but you will likely skip over or miss a step. It is important to actually DO and WRITE DOWN the steps as you do them, for the best result. -
Problem Solving
-
In this section you'll learn about a problem solving process called Goal-Plan-Do-Review (GPDR).GPDR has been used successfully for many years in rehabilitation work with individuals who have sustained a brain injury. Now you have an opportunity to use this proven strategy at home with your family member.
Step 1: Identify the Issue
What is the issue or behavior that is creating tension or anxiety in your family?
State the issue in a way that is:
- specific and
- neutral.
Using neutral language – just saying what you see, not how you feel about it, can help identify the real issue and lead to real solutions.
Examples:
NOT – He's lazy and won’t get off the couch!
BUT – He has a hard time starting a new activity.NOT – She's so stubborn.
BUT – She has a hard time with change.Step 2: Set the Goal
After you have described the issue in clear, neutral language, the next step is to state what you and your family member want to change: the goal.
What do you and your loved one want to change?
To set a goal, keep these things in mind:
- Focus on one goal at a time
- Pick something that is do-able
- Use clear, objective language to describe the goal
Example:
Behavior: When David doesn’t get out of bed on time in the morning, he is angry the rest of the day.
Goal: David will remember to get out of bed when his alarm goes off in the morning.Step 3: Make a Plan
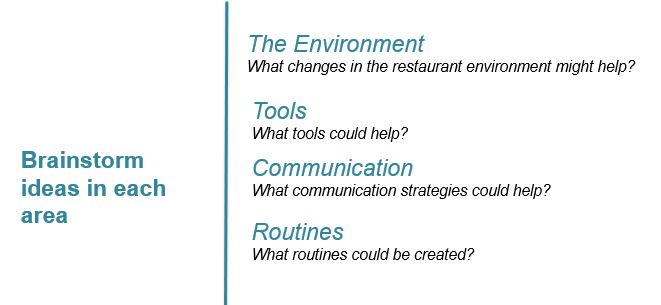
You've been introducted to strategies designed to give you ideas for how to make changes in your home environment, strategies around using tools (e.g., lists, schedules, and routines), and strategies for using effective communication. Now select a few strategies and make your plan!
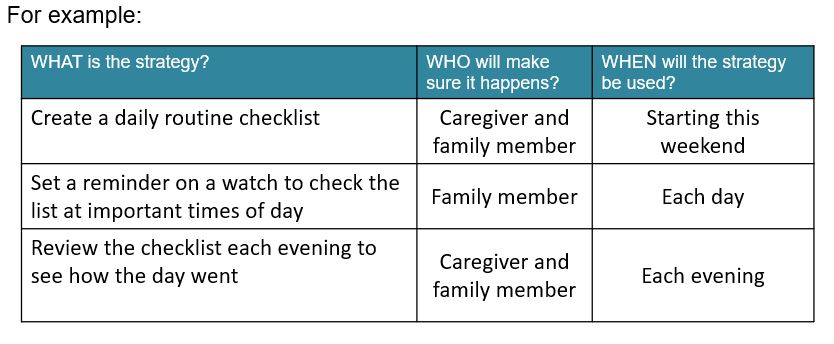
Be sure to include
WHAT: Start with a few strategies.
WHO: Determine who will do them.
WHEN: Set a time that you will start.Step 4: Do the Plan
Once everyone involved agrees on a plan, set the plan in motion and see it through. Things may not be perfect, but if there is improvement, keep it going. Expect it to work some or most of the time, not all of the time.
Be a good coach! Offer encouragement. | Keep the plan on track. | Be patient – it may take a few triesStep 5: Review the Plan
Check in together as a family from time to time to see how the plan is working, not just for the person with a brain injury but also for the other family members as well. This is an important step that is often overlooked.
What worked? | What didn’t work? | What could we do differently?Final thoughts from Dr. Feeney.